In the COADAPT project, FIOH (Finnish Institute of Occupational Health) investigates whether the use of smart shift scheduling software among the ageing workers in the health and social care sector will support their health and workability. The intervention study has already been finalized and the first scientific paper of the results on sleep and workability is under review.
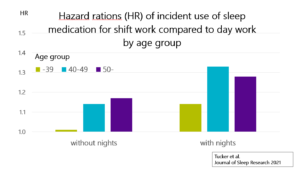
In the COADAPT project, we started by analyzing the overall associations of ageing with health and well-being in shift work. As part of this research, a new paper was published recently on the association of rotating shift work, ageing and sleep. More specifically, we examined whether working rotating shifts, with or without night work, is associated with the purchase of prescribed sleep medication, and whether this association is dependent on age. Data were obtained from a longitudinal cohort study of Finnish public sector employees who responded to questions on work schedule and background characteristics in 2000, 2004 and 2008. The data were linked to national register data on redeemed prescriptions of hypnotic and sedative medications, with up to 11 years of follow-up. Age stratified Cox proportional hazard regression models were computed to examine incident use of medication comparing two groups of rotating shift workers (those working shifts that included night shifts and those whose schedules did not include night shifts) with day workers who worked in a similar range of occupations.
Elderly rotating shift workers already after 40 years were more likely to purchase prescribed hypnotic and sedative medication than their day-working counterparts
The results showed that shift work with night shifts was associated with increased use of sleep medication in all age groups, after adjustments for sex, occupational status, marital status, alcohol consumption, smoking and physical activity levels (hazard ratio [HR], [95% confidence interval, CI] 1.14 [1.01–1.28] for age group ≤39 years; 1.33 [1.19–1.48] for age group 40–49 years; 1.28 [1.13–1.44] for age group ≥50 years). Shift work without nights was associated with medication use in only the two older age groups (HR [95% CI] 1.14 [1.01–1.29] and 1.17 [1.05–1.31] for age groups 40–49 years and >50 years, respectively).
Conclusions in relation to ageing
The findings suggest that circadian disruption and older age, already after the age of 40 years, puts rotating shift workers, and especially those who work nights, at increased risk of developing clinically significant levels of sleep problems. In relation to the COADAPT aims, the elderly workers would thus probably benefit most from any interventions decreasing sleep disorders.
Link to the original publication
Tucker P, Härmä M, Ojajärvi A, Kivimäki M, Leineweber C, Oksanen T, Salo P, Vahtera J. Association of rotating shift work schedules and the use of prescribed sleep medication: A prospective cohort study. J Sleep Res. 2021 Jun 14:e13349. Online ahead of print. doi: 10.1111/jsr.13349.